What Is Fatty Liver: Causes, Symptoms, and Treatment
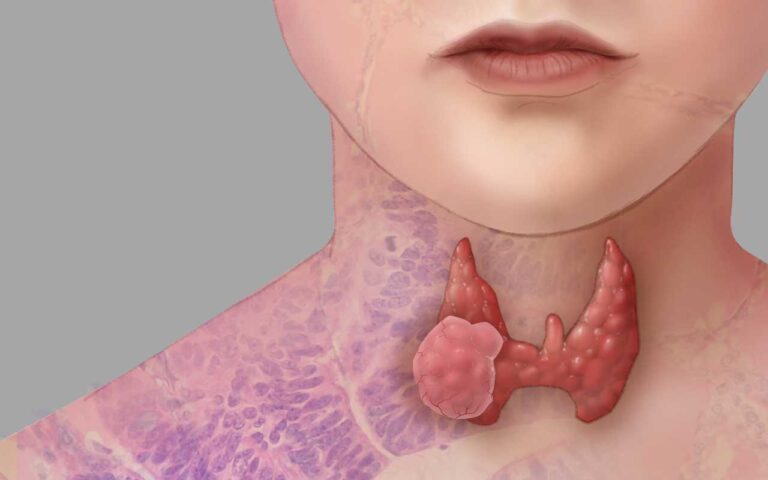
Fatty Liver: The liver is one of the most vital organs in the human body, responsible for processing nutrients, detoxifying harmful substances, and producing bile, which aids in digestion. However, when fat accumulates in the liver cells beyond normal levels, it can lead to a condition known as fatty liver, or hepatic steatosis. Fatty liver is a common but often under-recognized condition that can have serious health consequences if left unmanaged. This article will explore the causes, symptoms, and treatment options for fatty liver, providing a comprehensive overview for those seeking to understand this condition better. (liver disease fatty liver)
What is Fatty Liver?
Fatty liver occurs when more than 5-10% of the liver’s weight is fat. It is generally classified into two types: (fatty liver problem)
- Alcoholic Fatty Liver Disease (AFLD): This type is directly related to heavy alcohol consumption. The liver metabolizes alcohol, but excessive amounts can lead to fat buildup, inflammation, and eventually scarring of the liver tissue.
- Non-Alcoholic Fatty Liver Disease (NAFLD): This occurs in people who consume little to no alcohol. NAFLD is becoming increasingly prevalent, especially in Western countries, and is closely linked to metabolic syndrome, obesity, insulin resistance, and type 2 diabetes.
Causes of Fatty Liver
Understanding the causes of fatty liver is crucial for prevention and management. While the exact mechanisms are not entirely understood, several factors contribute to the development of this condition:
- Alcohol Consumption:
- AFLD is primarily caused by chronic alcohol abuse. The liver processes alcohol into substances that are more harmful than alcohol itself, leading to liver damage and fat accumulation.
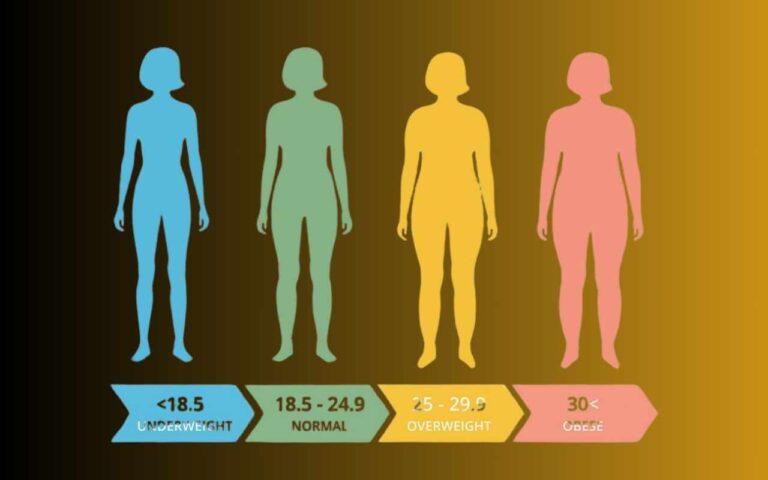
- Obesity:
- Obesity, particularly abdominal obesity, is a major risk factor for NAFLD. Excess body fat, particularly visceral fat, can lead to insulin resistance, which in turn promotes fat storage in the liver.
- Insulin Resistance and Type 2 Diabetes:
- Insulin resistance, a hallmark of type 2 diabetes, is closely linked to NAFLD. When cells become resistant to insulin, the liver responds by producing more glucose and fat, contributing to fat accumulation in the liver.
- High Cholesterol and Triglycerides:
- Elevated levels of cholesterol and triglycerides in the blood can contribute to fat buildup in the liver. This is often seen in people with metabolic syndrome, a cluster of conditions that increase the risk of heart disease, stroke, and type 2 diabetes.
- Genetics:
- Genetic factors may play a role in the development of fatty liver. Certain gene mutations, such as PNPLA3, have been associated with an increased risk of NAFLD.
- Diet and Lifestyle:
- A diet high in refined carbohydrates, sugars, and unhealthy fats can contribute to liver fat accumulation. A sedentary lifestyle and lack of physical activity further exacerbate the risk.
- Medications:
- Some medications, such as corticosteroids, tamoxifen, and certain antidepressants, can contribute to fatty liver development by promoting fat accumulation in the liver.
Symptoms of Fatty Liver
Fatty liver is often called a “silent” disease because it may not cause noticeable symptoms, especially in the early stages. However, as the condition progresses, some symptoms may appear, including: (Fatty liver causes)
- Fatigue:
- Persistent tiredness and lack of energy are common symptoms. The liver’s reduced efficiency in processing nutrients and detoxifying the body can contribute to overall fatigue.
- Abdominal Discomfort:
- Some individuals may experience dull or aching pain in the upper right abdomen, where the liver is located. This discomfort is usually due to the enlarged liver pressing against surrounding tissues.
- Weight Loss and Muscle Weakness:
- Unexplained weight loss and muscle weakness can occur as the liver becomes less effective at metabolizing fats and proteins.
- Jaundice:
- In more severe cases, jaundice, or yellowing of the skin and eyes, may develop. This occurs when the liver’s ability to process bilirubin, a waste product from the breakdown of red blood cells, is impaired.
- Swelling and Fluid Retention:
- Advanced fatty liver can lead to fluid retention, particularly in the abdomen (ascites) and legs (edema), due to reduced liver function and protein production.
- Mental Confusion:
- In severe cases, fatty liver can progress to hepatic encephalopathy, a condition characterized by confusion, forgetfulness, and difficulty concentrating due to the buildup of toxins in the brain.

Diagnosis of Fatty Liver
Diagnosing fatty liver typically involves a combination of medical history, physical examination, and diagnostic tests:
- Blood Tests:
- Liver function tests (LFTs) can detect elevated liver enzymes, which may indicate liver inflammation or damage. However, normal liver enzyme levels do not rule out fatty liver.
- Imaging Studies:
- Ultrasound is the most common imaging technique used to diagnose fatty liver. It can detect the presence of fat in the liver, though it cannot differentiate between AFLD and NAFLD.
- MRI and CT scans provide more detailed images and can quantify the amount of fat in the liver.
- Liver Biopsy:
- In some cases, a liver biopsy may be performed to confirm the diagnosis and assess the extent of liver damage. A small tissue sample is taken from the liver and examined under a microscope.
Treatment of Fatty Liver
The treatment of fatty liver focuses on addressing the underlying causes and preventing the progression of liver damage. There is no specific medication to cure fatty liver, but several strategies can help manage and reverse the condition: (Fatty liver treatment)
- Lifestyle Modifications:
- Weight Loss:
- For individuals with NAFLD, gradual weight loss is one of the most effective ways to reduce liver fat. A loss of 7-10% of body weight can significantly improve liver health.
- Diet:
- Adopting a balanced diet low in saturated fats, refined sugars, and processed foods is crucial. The Mediterranean diet, rich in fruits, vegetables, whole grains, and healthy fats, is often recommended for fatty liver patients.
- Exercise:
- Regular physical activity, such as aerobic exercise and resistance training, helps improve insulin sensitivity, reduce liver fat, and promote overall health.
- Weight Loss:
- Alcohol Abstinence:
- For those with AFLD, complete abstinence from alcohol is essential to prevent further liver damage and allow the liver to heal.
- Medications:
- Although there is no specific medication for fatty liver, certain drugs may be prescribed to manage associated conditions such as insulin resistance, high cholesterol, and diabetes. For example, metformin, pioglitazone, and statins may be used in certain cases.
- Vitamin E Supplementation:
- Some studies suggest that vitamin E, an antioxidant, may help reduce liver inflammation and damage in people with NAFLD. However, this treatment should be discussed with a healthcare provider, as high doses of vitamin E can have side effects.
- Bariatric Surgery:
- For individuals with severe obesity and NAFLD who do not respond to lifestyle changes, bariatric surgery may be considered. Weight loss surgery can lead to significant improvements in liver health.
- Monitoring and Follow-Up:
- Regular monitoring of liver function and overall health is crucial for individuals with fatty liver. Follow-up visits with a healthcare provider can help track progress, make necessary adjustments to the treatment plan, and detect any complications early. (liver problems fatty)
The Importance of Regular Health Screening
Life expectancy with fatty liver disease
Life expectancy with fatty liver disease varies based on the type and severity of the condition. For those with simple NAFLD (non-alcoholic fatty liver disease), life expectancy may not be significantly impacted if managed with lifestyle changes. However, if the disease progresses to NASH (non-alcoholic steatohepatitis), which involves liver inflammation and damage, the risk of developing cirrhosis or liver cancer increases, potentially shortening life expectancy.





One Comment